TL;DR
|
In healthcare, every minute lost to inefficiency costs more than time; it costs care.
Across hospitals, clinics, and care networks, operational inefficiencies have become silent drains on profits. From high call volumes to delayed documentation and manual scheduling, the administrative load is consuming resources that could be allocated to patient care.
Studies show that missed medical appointments alone cost the U.S. healthcare system over $150 billion annually, with no-show rates ranging from 5% to 30%, depending on the practice type. At the same time, administrative costs now account for nearly 25 % of total healthcare spending, much of it tied to manual, repetitive tasks.
While technology has long promised to fix these inefficiencies, many organizations still struggle to quantify the real return on investment (ROI).
Leaders are asking hard questions: How much time can automation actually save? How quickly will it pay for itself? What measurable outcomes justify the shift?
This is where a structured ROI framework becomes essential. Understanding where your organization loses time, how automation impacts performance, and which levers drive measurable value can turn technology investment into tangible financial and clinical gains.
In this blog, we break down the fundamental ROI drivers for healthcare automation, from cost savings and revenue protection to clinical efficiency and staff satisfaction. You’ll also learn how to model ROI step by step, evaluate costs and risks, and build a solid financial case for technology adoption.
TL;DR
|
The Voice AI Revolution: Beyond Automation to Conversational Infrastructure
Voice is the most natural form of communication. It does not require technical training, manual input, or screen interaction. This makes it especially well-suited for healthcare, where users, patients, providers, and administrative staff are often under time pressure or may have varying levels of digital literacy.
For patients, speaking is far more accessible than navigating websites or apps. For staff, voice-based systems reduce the need to multitask between devices and screens, allowing for a more seamless workflow. This simplicity leads to higher adoption rates and lower friction in day-to-day operations.
Moving Beyond Conventional IVRs and Chatbots
AI voice agents differ from Interactive Voice Response (IVR) systems and basic scripted chatbots. The difference lies in capability, adaptability, and contextual understanding:
| Feature | IVR / Chatbots | AI Voice Agents |
| Response Type | Menu-based or keyword-triggered | Conversational and dynamic |
| Availability | Limited or fixed-hour scripts | 24/7, always-on |
| Context Understanding | No contextual memory | Remembers context within interactions |
| Flexibility | Predefined flows only | Can handle open-ended queries |
| Escalation | Manual handover needed | Can auto-escalate based on confidence or rules |
| Personalization | Generic responses | Adapted to user history or input |
AI voice agents understand natural language, follow multi-turn conversations, adapt to changing input, and handle interruptions, making them suitable for real-time patient interaction and support.
Why Is This the Right Time for Adoption?
Several technological advancements have matured simultaneously, making AI voice agents reliable and viable for healthcare applications:
- Automatic Speech Recognition (ASR): Improved accuracy even in noisy environments and with diverse accents.
- Natural Language Understanding (NLU): Ability to interpret medical terms, understand patient intent, and differentiate between routine and urgent needs.
- Text-to-Speech (TTS): More natural and empathetic voice output enhances user trust and comfort.
- Healthcare-Specific AI Training: Voice agents can now be trained on clinical workflows, terminology, and compliance standards, such as HIPAA.
- Cloud Infrastructure & API Integrations: Easy deployment with existing Electronic Health Records (EHRs), CRM systems, and call center platforms.
These advancements reduce implementation risks and increase performance reliability, enabling healthcare providers to scale operations without compromising service quality.
AI voice agents should not be viewed as simple automation tools. Instead, they are becoming core infrastructure, capable of supporting multiple workflows across scheduling, triage, patient communication, documentation, and follow-up care.
Their modularity enables them to serve different departments while drawing from a shared knowledge base. This creates consistency in communication, improves data capture, and enhances operational efficiency across the organization.
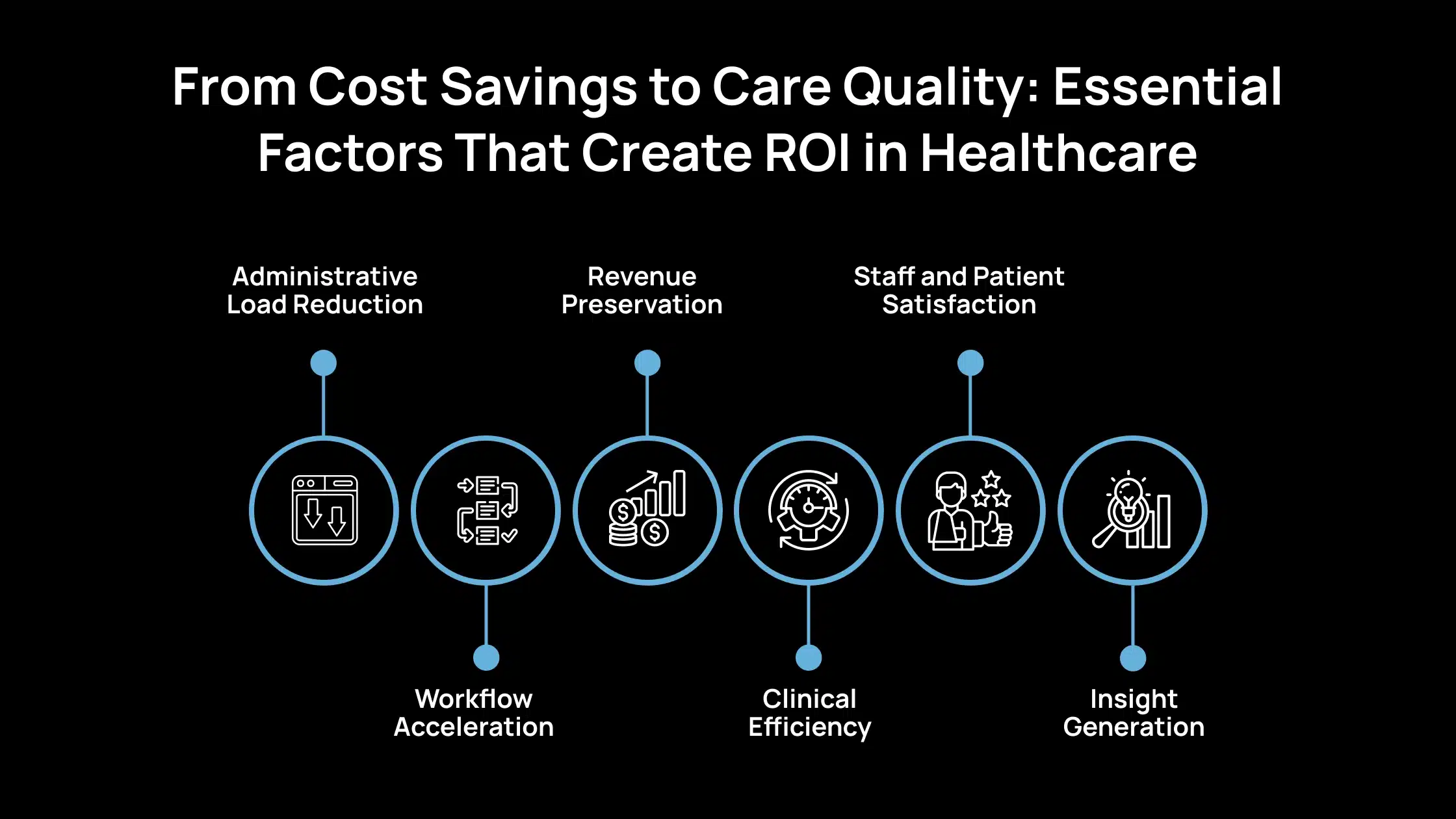
From Cost Savings to Care Quality: Essential Factors That Create ROI in Healthcare
ROI in healthcare operations isn’t a single number; it’s the outcome of several measurable factors that improve efficiency, reduce costs, and enhance overall performance. Below are the essential components that drive real, sustained ROI:
1. Administrative Load Reduction
Automating repetitive call center tasks such as appointment confirmations, insurance verification, and routine inquiries significantly reduces manual effort. This enables administrative teams to focus on higher-value tasks, such as patient engagement and issue resolution, thereby improving both accuracy and productivity.
2. Workflow Acceleration
AI-driven systems enable faster patient triage, documentation, and routing. By minimizing delays between intake, assessment, and follow-up, healthcare providers can serve more patients in a shorter timeframe. Streamlined workflows also reduce bottlenecks, helping teams maintain operational efficiency even during peak hours.
3. Revenue Preservation
Reducing appointment no-shows through automated reminders and follow-ups helps prevent lost revenue opportunities. Additionally, improved billing adherence, enabled by accurate documentation and timely claim submissions, ensures steady cash flow and fewer denials.
4. Clinical Efficiency
With ambient scribing and post-visit automation, clinicians spend less time on paperwork and more time on direct patient care. Automated note-taking and record updates enhance data accuracy while reducing administrative overhead, thereby improving both care quality and efficiency.
5. Staff and Patient Satisfaction
By reducing repetitive workloads and streamlining communication, automation helps prevent staff burnout and improves morale. For patients, timely responses and personalized care create a smoother experience, strengthening trust and satisfaction across every interaction.
6. Insight Generation
Each automated interaction generates valuable data on patient behavior, call volume trends, and operational performance. These insights enable healthcare leaders to make informed decisions, identify areas for improvement, and continually refine processes for better outcomes.
Tracking Performance: The Most Important ROI KPIs in Healthcare
Below are the key metrics and KPIs that help healthcare organizations measure the true ROI and performance impact of AI voice agents.
| Metric / KPI | Description |
| Call Deflection Rate | Share of calls resolved by automation without human help. |
| Average Handling Time (AHT) / Wait Time | Measures time saved per interaction through faster workflows. |
| First Contact Resolution (FCR) | Percentage of issues resolved in the first interaction. |
| No-Show Rate Reduction | Tracks decrease in missed appointments via automated reminders. |
| Clinical Documentation Time Saved | Time saved by providers through automated scribing or notes. |
| Cost per Interaction | Average cost to handle each patient interaction. |
| NPS / CSAT Change | Reflects improvement in patient satisfaction and loyalty. |
| Revenue Leakage Prevented / Collections | Revenue increased due to fewer billing errors and fewer missed payments. |
| ROI Payback Period | Time needed to recover the investment from realized gains. |
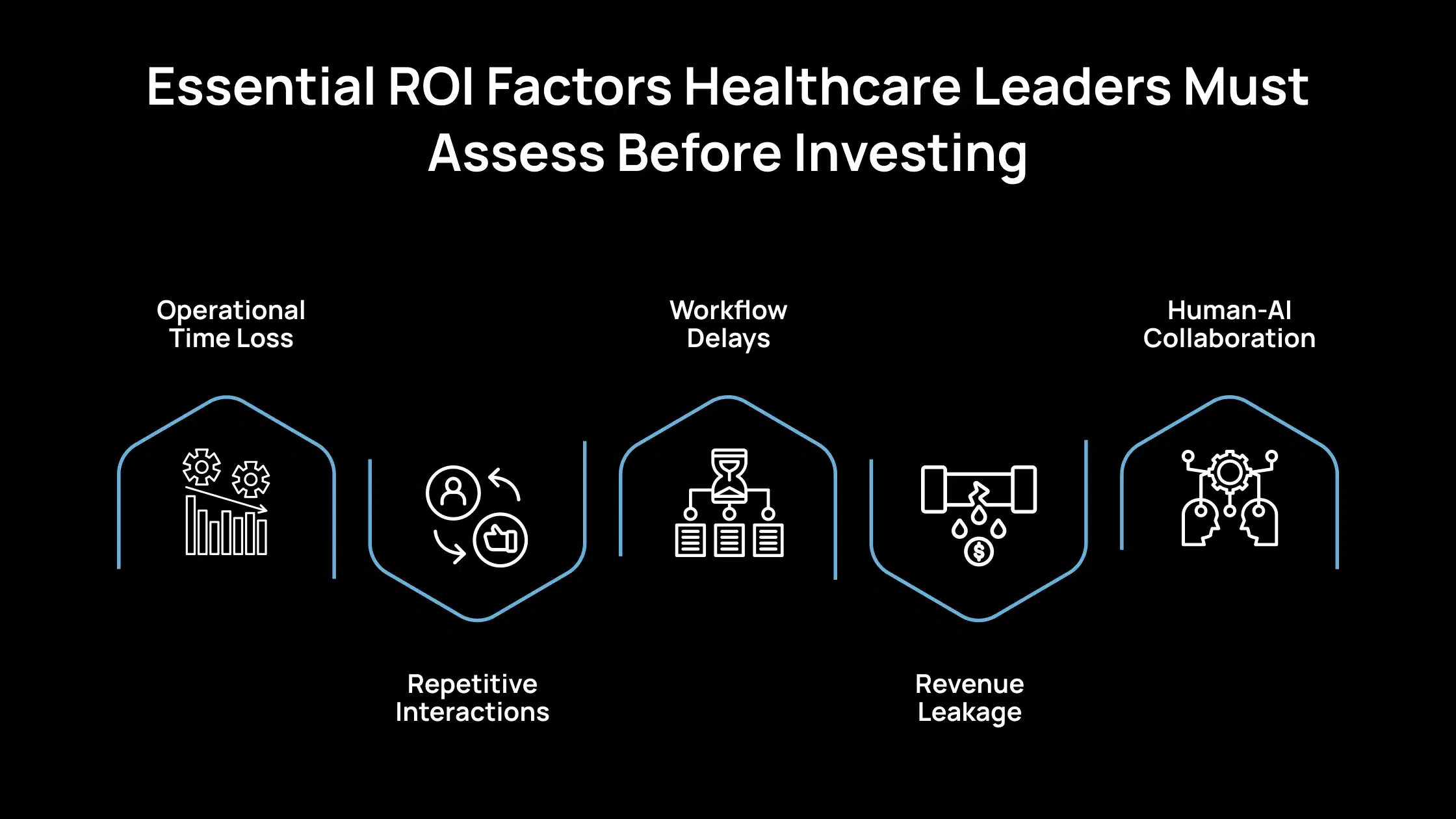
Essential ROI Factors Healthcare Leaders Must Assess Before Investing
Below are the essential ROI factors that healthcare decision-makers should review to make informed, value-driven investment decisions.
1. Operational Time Loss
Organizations often lose significant time handling routine communication tasks such as appointment confirmations, patient inquiries, and follow-up reminders. Identifying where these manual interactions consume the most time helps pinpoint areas where automation can create immediate efficiency gains.
2. Repetitive Interactions
A large portion of patient communication involves rule-based or repetitive exchanges, such as collecting standard patient information, sending reminders, or providing basic instructions. Recognizing these patterns helps determine which processes can be streamlined through automation without affecting the quality of care.
3. Workflow Delays
Manual triage and scheduling introduce delays that slow down the entire patient journey. Reducing human dependency in these steps, where appropriate, accelerates response times and enables faster care delivery, improving both operational flow and patient satisfaction.
4. Revenue Leakage
Missed appointments, incomplete follow-ups, and billing delays lead to measurable revenue loss. Understanding the financial impact of these inefficiencies is crucial for quantifying the potential return on investment in automated or AI-driven communication systems.
5. Human-AI Collaboration
The goal of voice automation is to support, not replace, clinical and administrative staff. Evaluating where voice technology can augment existing workflows, such as patient intake or documentation support, ensures that automation enhances human care rather than disrupts it.
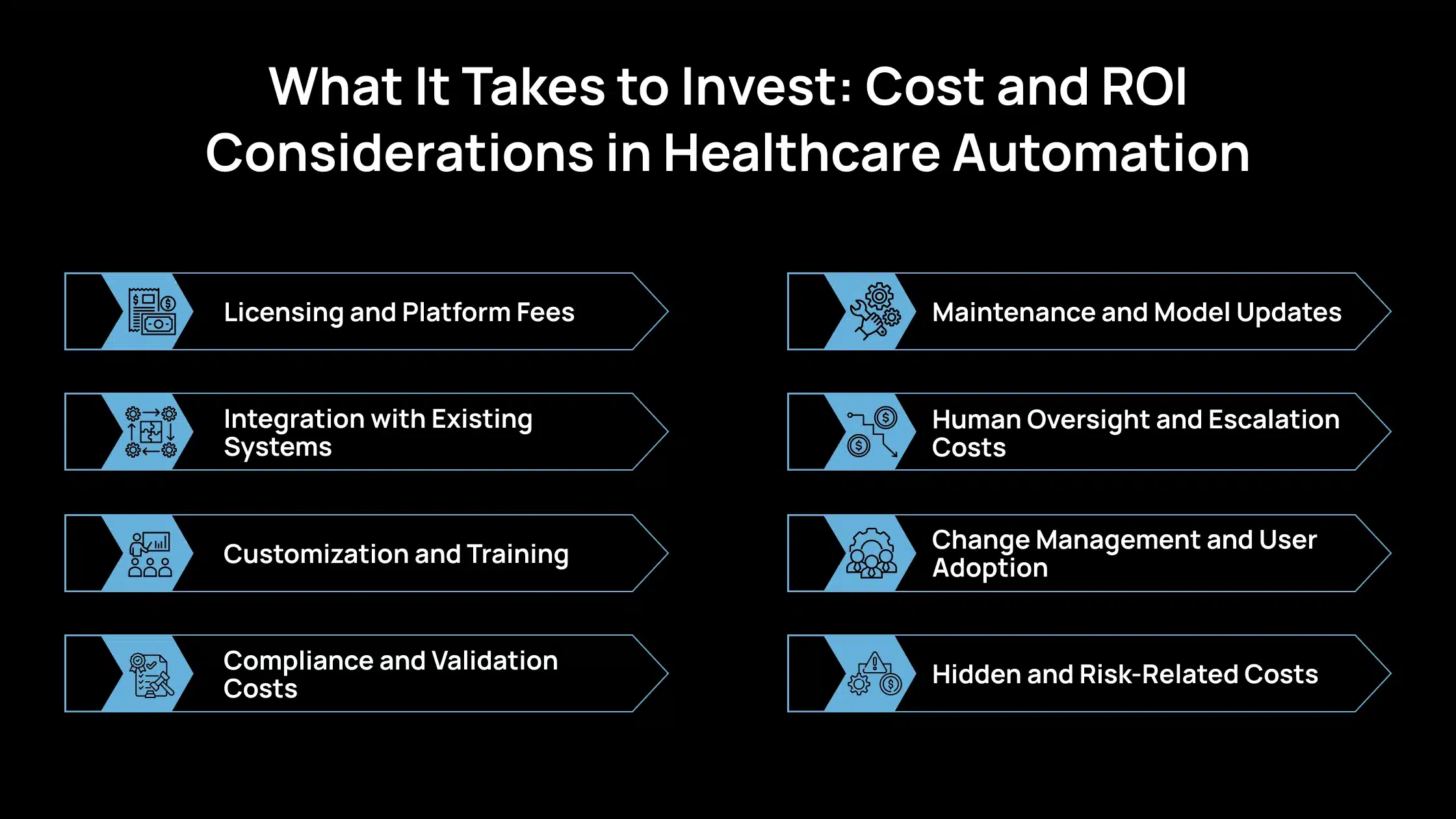
What It Takes to Invest: Cost and ROI Considerations in Healthcare Automation
Investing in AI-powered communication or automation systems requires careful financial planning beyond initial setup. Decision-makers should evaluate both direct and indirect costs to ensure sustainable ROI. Below are the essential cost and investment factors to consider:
1. Licensing and Platform Fees
Most AI and automation platforms require annual or usage-based licensing. These costs can vary based on the number of users, call volumes, or integration features. It’s important to understand pricing models early to avoid scalability issues later.
2. Integration with Existing Systems
Connecting new AI tools with EHRs, CRMs, and telephony platforms can be complex. Integration requires technical effort for data mapping, workflow alignment, and testing. These activities often involve one-time professional service fees.
3. Customization and Training
Each healthcare environment has unique communication needs. Customizing conversation flows, automating patient journeys, and training AI models demand specialized design and development time, which adds to upfront investment.
4. Compliance and Validation Costs
Healthcare systems must comply with HIPAA and other data protection standards. Ensuring secure data handling, auditing workflows, and validating model performance all require dedicated compliance resources.
5. Maintenance and Model Updates
Ongoing costs include hosting, software maintenance, and retraining the AI model to keep systems accurate and relevant. Regular updates are necessary to adapt to changes in policy, workflow, and technology.
6. Human Oversight and Escalation Costs
Even with automation, specific interactions require human intervention. Allocating staff for escalation handling, quality assurance, and exception management adds recurring operational expenses.
7. Change Management and User Adoption
Successful implementation depends on how well staff adapt to the new system. Training employees, addressing resistance to change, and maintaining engagement involve both time and cost.
8. Hidden and Risk-Related Costs
Potential risks, such as misrecognition, AI errors, or inaccurate responses, can lead to patient dissatisfaction or compliance breaches. These issues might result in financial penalties or additional remediation expenses.
ROI Modeling Blueprint: How to Build the Financial Case in Healthcare
Below are the critical cost and investment considerations healthcare leaders should evaluate to ensure sustainable ROI from AI voice agent implementation.
1. Define the Baseline
Begin by establishing the current state of operations. Capture key metrics such as call volumes, patient interactions, average handling times, staffing levels, and related costs. Include administrative workload, overtime, and technology expenses.
This baseline forms the foundation for measuring improvements in cost, efficiency, and care delivery.
2. Estimate Current and Target Performance
Assess the performance of agents and staff across communication channels, such as call centers, front-desk operations, and clinical documentation. Identify benchmarks like deflection rate, triage accuracy, and response times.
Then, estimate achievable performance targets with automation, such as reduced manual workload or improved data accuracy.
3. Map to Healthcare Value Streams
Translate improvements into tangible healthcare outcomes. Connect automation benefits to areas like reduced administrative costs, fewer missed appointments, faster patient intake, improved billing accuracy, and enhanced care coordination. Each improvement should align with measurable financial or operational gains.
4. Model Over Time (3–5 Year Horizon)
Project ROI over a multi-year period to account for adoption, training, and system maturity. Include implementation phases, learning curves, and technology scaling.
Healthcare systems often see increasing value over time as workflows stabilize and automation integrates more deeply with EHRs and clinical operations.
5. Conduct Sensitivity and Scenario Analysis
Test how different outcomes affect ROI under various conditions, such as patient volume fluctuations, staff adoption rates, or regulatory changes.
Scenario analysis helps identify the factors that have the most significant impact on financial results and prepares leadership for best-case, expected, and risk-adjusted outcomes.
6. Identify Significant Operational Points
Identify areas where small operational changes can yield significant financial or clinical benefits. For example, even a slight drop in patient no-shows, a small improvement in triage speed, or a modest reduction in documentation time per visit can significantly improve ROI. These utilization points help prioritize optimization and ongoing investment.
How AI Voice Agents Benefit Your Healthcare Organization
In healthcare, every missed call can mean a missed appointment, a delayed treatment, or a lost patient opportunity. The Avahi AI Voice Agent helps healthcare organizations ensure that no patient call goes unanswered, even after hours, on weekends, or during peak times.
Built on secure AWS infrastructure, this always-on solution manages patient calls efficiently and reliably. It can schedule appointments, verify information, route calls to the correct department, or hand off to a live staff member when needed, all while maintaining HIPAA-compliant communication standards.
Essential Benefits for Healthcare Providers
- Reduce Missed Appointments: Automated confirmations and reminders minimize no-shows and keep schedules full.
- Enhance Patient Access: Handle high call volumes without additional staff, ensuring patients reach the right care channel quickly.
- Improve Staff Productivity: Let the AI manage routine calls and data entry, freeing clinical and administrative teams to focus on patient care.
- Deliver 24/7 Availability: Provide consistent patient communication — no more after-hours gaps, voicemail delays, or long hold times.
- Boost Patient Satisfaction: Offer quick, accurate, and empathetic responses that improve overall patient experience.
- Ensure Data Security and Compliance: Built on AWS with encryption and audit controls, the system supports healthcare-grade reliability and compliance.
- Gain Actionable Insights: Access real-time call data and analytics to identify trends, streamline workflows, and optimize patient engagement strategies.
The Avahi AI Voice Agent empowers healthcare organizations to provide faster, more reliable patient communication, improving efficiency, reducing costs, and strengthening patient trust at every interaction.
Discover Avahi’s AI Platform in Action
At Avahi, we empower businesses to deploy advanced Generative AI that streamlines operations, enhances decision-making, and accelerates innovation—all with zero complexity.
As your trusted AWS Cloud Consulting Partner, we empower organizations to harness the full potential of AI while ensuring security, scalability, and compliance with industry-leading cloud solutions.
Our AI Solutions Include
- AI Adoption & Integration – Utilize Amazon Bedrock and GenAI to Enhance Automation and Decision-Making.
- Custom AI Development – Build intelligent applications tailored to your business needs.
- AI Model Optimization – Seamlessly switch between AI models with automated cost, accuracy, and performance comparisons.
- AI Automation – Automate repetitive tasks and free up time for strategic growth.
- Advanced Security & AI Governance – Ensure compliance, detect fraud, and deploy secure models.
Want to unlock the power of AI with enterprise-grade security and efficiency? Start Your AI Transformation with Avahi Today!
Frequently Asked Questions
1. What is the ROI of AI voice agents ROI in healthcare?
The ROI of AI voice agents in healthcare measures the financial and operational returns gained from implementing AI-powered voice systems. It includes cost savings, reduced administrative load, improved patient communication, and higher staff efficiency.
2. How can hospitals calculate AI voice agents’ ROI in healthcare?
Hospitals can calculate the ROI of AI voice agents in healthcare by comparing pre- and post-implementation data, such as call volume handled, appointment adherence, documentation time saved, and cost per interaction. Tracking these metrics helps quantify real financial impact.
3. What factors influence AI voice agents’ ROI in healthcare?
The ROI depends on automation coverage, integration with EHR and CRM systems, call deflection rates, clinical documentation efficiency, and patient satisfaction. Strong adoption and optimized workflows maximize returns.
4. How quickly can healthcare organizations see ROI from AI voice agents?
Most healthcare providers begin to see measurable ROI from AI voice agents within 6–12 months, depending on scale, workflow complexity, and implementation readiness. Gradual improvements in efficiency and revenue recovery compound over time.
5. Why is measuring AI voice agents’ ROI in healthcare important?
Measuring the ROI of AI voice agents in healthcare ensures that technology investments align with strategic goals. It helps justify costs, identify performance gaps, and demonstrate clear value in operational and clinical outcomes.